A new study by a US-based research group has shown that imaging of the mouse brain using Functional Ultrasound (fUS) and Ultrasound Localization Microscopy (ULM) can help to explain why cognitive function can decline following treatment with the chemotherapy drug paclitaxel.
Chemotherapy-induced cognitive impairment (CICI), also referred to as ‘chemobrain’, affects 30–50% of chemotherapy patients, and causes loss of memory, attention and executive function, which can be long-lasting. CICI was originally believed to be caused by the toxicity of chemotherapy drugs to neurons, but there are increasing indications that effects on the brain’s vascular network play a key role.
Using brain imaging equipment supplied by Iconeus, researchers at the University of Oklahoma Health Sciences Center in Oklahoma City, USA, have now found evidence suggesting that cerebrovascular dysfunction contributes to CICI. Their work involved administering the widely-used chemotherapy drug paclitaxel to mice in two cycles separated by a 1-week interval. This was followed after 6 months by whole-brain imaging through a polymeric window using an Iconeus One fUS system.
High-resolution insights from fUS and ULM brain imaging
The work carried out by the researchers focused on two imaging protocols available using Iconeus One.
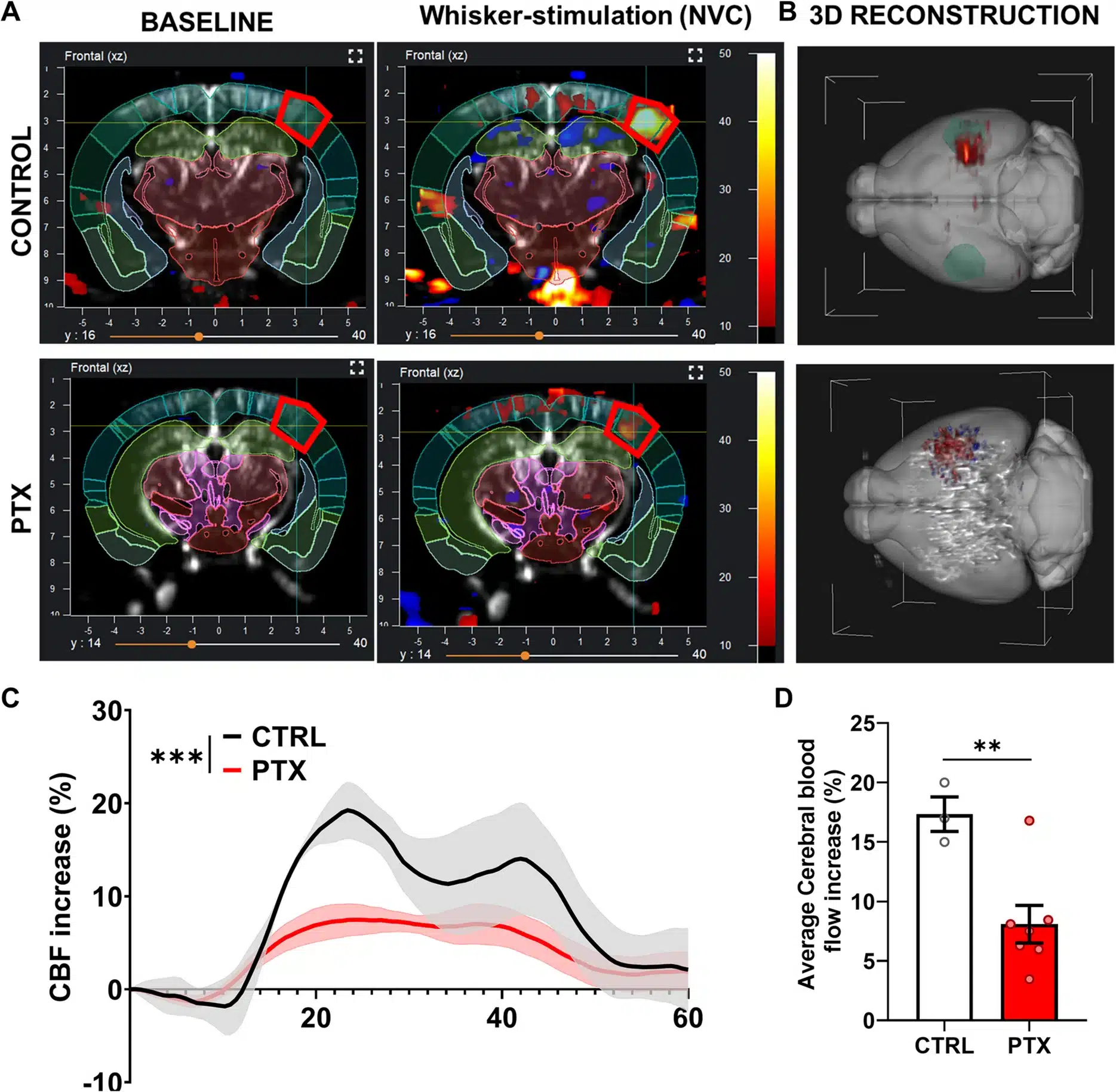
Firstly, regular functional ultrasound (fUS) provided information on the neurovascular responses in response to whisker stimulation, with the amplitude of cerebral blood flow changes found to be “markedly smaller” in paclitaxel-treated animals compared to controls.
Secondly, the microbubble-enabled Ultrasound Localization Microscopy (ULM) technique provided high-resolution data on microvascular density. The researchers say that the paclitaxel treatment led to a “sustained reduction” in microvascular density within the cerebral cortex and hippocampus, two regions that are important for higher cognitive functions, including learning and memory.
The ULM study also provided information on mean blood flows. In mice treated with paclitaxel, they say “the cumulative average blood velocity in the middle cerebral arteries decreased significantly”. This, the researchers point out, is consistent with the idea that there is a link between impaired brain perfusion and the development of CICI.
Improved resolution for non-invasive whole-brain imaging
The authors say that the impaired neurovascular coupling responses, long-lasting reductions in microvascular density, and altered cerebral blood flows induced by paclitaxel demonstrate that it “induces persistent microvascular dysfunction that likely underlies CICI”. They go on to highlight the therapeutic potential of targeting vascular health in order to preserve cognitive function in cancer survivors.
From an experimental standpoint, they have positive comments on the utility of the fUS and ULM techniques, pointing out their non-invasiveness and superior spatiotemporal resolution. They are also impressed with the ability to carry out whole-brain imaging in the mouse in one session, saying that “Unlike traditional imaging techniques such as fMRI or two-photon microscopy, fUS enables detailed longitudinal assessment of cerebral vasculature across the entire brain”.
Towards a deeper understanding of drug–brain interactions
Having established the effect of paclitaxel in this study, the authors then point out the prospects for further work. Specifically, they suggest that future studies could use tumor-bearing mice rather than tumor-free strains, which were used here to eliminate confounding factors in the experiments. In addition, they recommend that fUS and ULM imaging studies should be carried out alongside behavioral and cognitive assessments, to establish a direct correlation between vascular dysfunction and cognitive impairment.
Ludovic Lecointre, Pharm.D., CEO and co-founder of Iconeus, congratulates the authors on their research, and says that it is an excellent example of the value of fUS and ULM imaging techniques: “The article from the Oklahoma team provides compelling evidence that chemotherapy can affect brain microcirculation and function, with implications for recovery of cancer survivors. It also is a powerful demonstration of the resolution that’s possible with the Iconeus One system, both in terms of functional responses and for direct vascular visualization – and we look forward to hearing about further work in this area”.
Reference:
S.S. Chandragiri, A. Nyul-Toth, S. Negri, R. Patai, R. Gulej, B. Csik, S. Shanmugarama, K.V. Kordestan, M. Nagykaldi, P. Mukli, A. Ungvari, A. Yabluchanskiy, Z. Ungvari, S. Tarantini and A. Csiszar, Functional ultrasound imaging reveals microvascular rarefaction, decreased cerebral blood flow, and impaired neurovascular coupling in a mouse model of paclitaxel-induced chemobrain, GeroScience, 2025, https://doi.org/10.1007/s11357-025-01624-7.